John worked in retail, but couldn’t communicate effectively with customers and relied mostly on lip-reading. He also couldn’t use the phone and had no email account, so if he wanted to communicate with people at his job or in our clinic—to ask a question or make a schedule change, for example—he rode his bike to the store or clinic to communicate face-to-face. His social communication suffered, and family members often became frustrated with his inability to take part in conversations.
Our clinic’s multidisciplinary aural rehabilitation program brings together audiology and speech-language graduate students to help patients, like John, with their CIs. Collaboration between a speech-language pathologist and an audiologist is common practice in aural rehabilitation for children with hearing loss, but the same is not typically true for adults.
The program improves outcomes for patients—measured in speech perception and quality-of-life assessments—and also benefits the student clinicians, as determined in pre- and post-clinic surveys about their understanding of the role of each profession in aural rehabilitation.
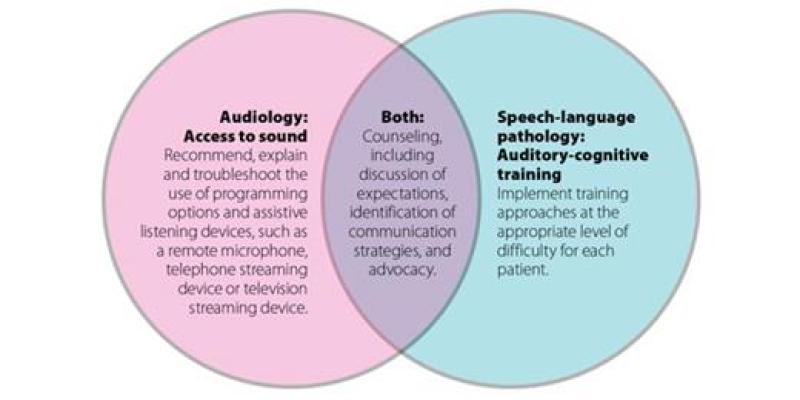
Audiology and speech-language pathology students are often so focused on learning within their respective programs that they overlook how complementary their skills really are, especially when treating patients with hearing-related communication difficulties. While audiologists specifically have expertise in managing hearing loss from an audibility standpoint, SLPs are skilled in scaffolding the learning required for auditory training. Students in both programs regularly focus on maximizing communication efficiency, so when both professions come to the table, students walk away with a holistic view of communication, and patient outcomes are optimized.
Students in both programs regularly focus on maximizing communication efficiency, so when both professions come to the table, students walk away with a holistic view of communication and patient outcomes are optimized.
Getting ready
Each semester, an audiology and speech-language pathology graduate student are paired together and assigned to the aural rehabilitation rotation. Their day of orientation includes:
Information from a surgeon on cochlear implants and patient communication outcomes.
An overview of aural rehabilitation by audiology and speech-language pathology preceptors that includes the rationale for aural rehabilitation as well as procedures, resources and expectations.
Hands-on training and troubleshooting with CIs and assistive listening devices with a CI manufacturer representative.
Working with the patients’ files and the guidance of the professionals, the team begins working together to develop treatment plans. The CI surgeon has a strong interest in patient success and refers any patients who report suboptimal outcomes to the program.
Goals and roles
When a patient who needs aural rehabilitation is referred to the clinic, we have a team of audiology students, speech-language pathology students and supervisors ready. The team establishes individualized hearing-related goals for the patient and develops a comprehensive plan of care, which typically includes managing expectations, assisting with devices and accessories, and providing auditory training and communication counseling. The ultimate goal for aural rehabilitation is to facilitate patients’ compliance with homework and recommendations, and to improve patients’ hearing-related quality of life.
Student clinicians also have goals. We want them to experience working with patients with CIs and hearing loss, gain a holistic view of communication, and recognize how collaboration affects patient outcomes.
In John’s case, audiology students took the lead in ensuring John understood his CI settings and how to use available assistive listening devices, such as a remote microphone and telephone streamer. Speech-language pathology students began auditory training, which included guided listening activities such as phoneme identification, sentence recognition in noise and listening comprehension.
Together, team members developed an individualized counseling blueprint. They asked John and members of his family to identify difficult listening situations, brainstorm contributing factors, define potential strategies or solutions, and plan how to best put strategies into action.
For example, John and his family identified communicating in a group of people as a top difficult-listening condition. The students provided general communication education and examples of case studies and research supporting effective communication strategies. With this support, John and his family agreed to implement three strategies:
John would ask for clarification as needed, and his wife and daughter agreed to position themselves so that John could see their faces when they spoke to him.
They identified the kitchen—with the ambient noise of appliances—as a difficult listening environment, and agreed to move conversations to the dining room.
They agreed to ensure proper lighting to enhance John’s ability to read lips.
The team incorporated aspects of each of these areas into every one-hour session for 10 weeks.
Value illustrated
At the end of 10 weeks, John had improved his sentence recognition scores in quiet and background noise, improved his scores on self-reported quality-of-life scales, successfully made phone calls using a telephone streamer, and reported general happiness with his performance and outlook on living with a CI.
All patient stories aren’t as picture-perfect as John’s, but all patients have reported an increased quality of life, even when sentence-recognition scores do not improve.
The comprehensive nature of the aural rehabilitation also results in positive student outcomes. They report increased knowledge of both audiology and speech-language pathology, as well as experience with collaboration that they can take with them into their professional careers.
“I now know the importance of the SLP in rehabilitating patients with hearing loss and the impact of interdisciplinary collaboration with audiology,” reports speech-language pathology graduate student Alexis Wilson after her experience in the aural rehabilitation clinic. “In the future, I will feel comfortable treating patients with hearing loss, collaborating with a team, and making appropriate referrals as needed.”
As research continues to demonstrate the benefit of multidisciplinary team care for patients, this clinical education experience sets the expectation for future clinicians that interprofessional practice is a fundamental feature of aural rehabilitation.